Heel pain is an incredibly common condition and there are very few Podiatrists who won’t see it on a daily basis in their clinics. There are numerous different causes of heel pain, (not all mechanical), but the area that this blog entry is going to focus on in particular is the plantar calcaneal/heel spur. It is yet another source of controversy, with no definitive agreement on the relationship of the spur and the surrounding tissues, or the actual source of the symptoms (if any) seen clinically.
Historically, it has been commonly accepted that heel spur formation is an abnormal finding and very closely correlated with the symptoms of heel pain. It was reported that excessive traction (pulling) of the plantar fascia on its attachment at the heel resulted in chronic inflammation, which in turn resulted in a reactive ossification and subsequent extra bone forming in the shape of a ‘spur’. 1-3 This is perhaps why heel spurs and ‘plantar fasciitis’ are still to this day thought by many to be one entity. Causation has been a point of confusion; does the traction and inflammation cause a heel spur, or does a heel spur cause tissue inflammation? A chicken and egg scenario. It is not uncommon to see statements that ‘plantar fasciitis’ is caused by heel spurs (admittedly this is on websites rather than academic journals), but is this factually correct?
The plantar calcaneal spur has been classically described as a bone outgrowth localised just anterior to the medial tuberosity of the calcaneus.4 This can not often be palpated clinically, but only seen radiologically as shown in the x-ray on the right above.
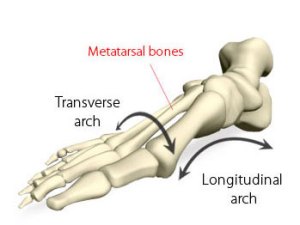
Another long term belief has been that individuals with heel pain are more likely to have pronated (flat) feet.5,6 As research has shown that lowering of the medial longitudinal arch of the foot increases plantar fascial tension7 it is easy to see how the connection between foot pronation, heel pain and heel spurs has been made. However the concern is that any individual who presents to a specialist with heel pain and ‘flat feet’ could be hastily assigned a diagnosis of “plantar fasciitis caused by a heel spur”. This is clearly unacceptable, and a specialist should have a much more thorough understanding of the research behind the pathological process. So, how common are heel spurs? Are they always problematic? Are they actually caused by traction? And what is their relationship with the plantar fascia?
How common are heel spurs?
Studies have shown that heel spurs are more common in pain free individuals than first thought, and it has been reported that anywhere between 11 and 27% of the population have radiographic evidence of a spur.5,8-13 Clearly this suggests they are not always associated with symptoms, and are not necessarily considered as ‘abnormal’ as once thought. Interestingly, even a study performed over 45 years ago on 323 patients concluded that the plantar calcaneal spur was never the cause of pain and probably a normal manifestation of the aging process.14
However, the research does suggest that calcaneal spurs do seem to be over-represented in certain groups, such as females,10,11,13 individuals with osteoarthritis15,16 and older people.11,13,15,16 Calcaneal spurs have also found to be more common in those who are overweight.17
Where are heel spurs?
As I have already mentioned, it has long been thought that heel spurs and plantar fascia problems were undeniably linked. Google ‘heel spurs’ and the term ‘plantar fasciitis’ is never far behind. However, it is interesting to hear how the anatomic studies report the actual location of the bony protrusion. Far from agreeing it resides solely within the plantar fascia as once thought, many studies found it can also be found above the plantar fascia.4,12,18 Some found it was much more commonly located in the other intrinsic musculature, (namely Flexor Digitorum Brevis and Abductor Digiti Minimi)4,18,19 and one study was as bold to firmly conclude that spurs do not develop within the plantar fascia.20
What is clear is that there is huge variability in the location of heel spur formation, and if we cannot unequivocally state that the spur is within the fascia (which we cannot) then the validity of its link with ‘plantar fasciitis’ is questionable.
What causes heel spurs?
As previously mentioned, the traditional theory for formation of plantar calcaneal spurs is what Menz and colleagues16 refer to as the longitudinal traction hypothesis, i.e. the plantar fascia pulling on the heel bone and causing the formation of a spur. Despite the anatomical studies showed that the spur is far from consistently found in the fascia, it has been suggested that there could be an element of tensile force exerted on the calcaneus from a variety of the other structures which attach to it.4,19
An alternative theory, termed the vertical compression hypothesis16 and was proposed by Kumai and Benjamin in 2002.20 This theory suggests that calcaneal spurs are outgrowths which form in response to repetitive vertical stress in an attempt to protect against microfractures. This idea is supported by histological studies which show that the bony trabeculae are NOT aligned in the direction of soft tissue traction.16,18 Li and Muehleman18 found that the direction of the trabeculae suggested that the force causing the pathological response was consistent with the external ground reaction force vector.
Conclusions
So what does all this mean in plain English? It means that we used to think a spur was caused by the plantar fascia pulling on the bone. This is highly unlikely as the spur is seldom found in the plantar fascia. If traction is the cause it is more likely to be caused by other musculature such as Flexor Digitorum Brevis or Abductor Digiti Minimi. However these bony protrusions could instead be caused by the repetitive vertical loading (the heel continuously hitting the floor, and the floor of course hitting it back) with the spur forming as a protective mechanism. Of course we cannot overlook the fact that there may be a combination of both traction and compression present in the aetiology of spur development. We also know that anywhere up to a quarter of the population may have a heel spur, but this will not always be problematic.
So, in summary:
The pathophysiology of plantar calcaneal heel spurs is poorly understood.
The presence of a plantar calcaneal spur does not always lead to the development of heel pain.
Plantar calcaneal spurs do appear to be associated with obesity, osteoarthritis and the aging process.
It is unclear whether spur formation is due to longitudinal traction of the plantar tissues or an adaptive response to vertical loading/compression (or both).
It is erroneous to assume there is a causal relationship between plantar calcaneal spurs and ‘plantar fasciitis’.
References
- DuVries, H.L. (1957). Heel spur (calcaneal spur). Archives of Surgery, 74: 536-542.
- Furey, J.G. (1975). Plantar fasciitis: the painful heel syndrome. Journal of Bone and Joint Surgery Am, 57: 672-673.
- Bergmann, J.N. (1990). History and mechanical control of heel spur pain. Clinics in Podiatric Medicine and Surgery, 7: 243-259.
- Abreu, M.R., Chung, C.B., Mendes, L. et al. (2003). Plantar calcaneal enthesophytes: new observations regarding sites of origin based on radiographic, MR imaging, anatomic, and paleopathologic analysis. Skeletal Radiology, 32: 13-21.
- Prichasuk, S., Subhadrabandhu, T. (1994). The relationship of pes planus and calcaneal spur to plantar heel pain. Clinical Orthopaedics and Related Research, 306: 192-196.
- Irving, D.B., Cook, J.L., Young, M.A. et el. (2007). Obesity and pronated foot type may increase the risk of chronic plantar heel pain: a matched case-control study. BMC Musculoskeletal Disorders, 8: 41.
- Kogler, G.F., Solomonidis, S.E., Paul, J.P. (1996). Biomechanics of longitudinal arch support mechanisms in foot orthoses and their effect on plantar aponeurosis strain. Clinical Biomechanics, 11: 243-252.
- Rubin, G., Witten, M. (1963). Plantar calcaneal spurs. American Journal of Orthopaedics, 5: 38-41.
- McCarthy, D.J., Gorecki, G.E. (1979). Anatomical basis of inferior calcaneal lesions: a cryomicrotomy study. Journal of the American Podiatric Medical Association, 69: 527-536.
- Shama, S.S., Kominsky, S.J., Lemont, H. (1983). Prevalence of non-painful heel spur and its relation to postural foot position. Journal of the American Podiatric Medical Association, 73: 122-123.
- Banadda, B.M., Gona, O., Vas, R., et al. (1992). Calcaneal spurs in a black African population. Foot & Ankle, 13: 352-354.
- Barrett, S.L., Day, S.V., Pignetti, T.T. et al. (1995). Endoscopic heel anatomy: analysis of 200 fresh frozen specimens. Journal of Foot & Ankle Surgery, 34: 51-56.
- Riepert, T., Drechsler, T., Schild, H. et al. (1996). Estimation of sex on the basis of radiographs of the calcaneus. Forensic Science International, 77: 133-140.
- Lapidus, P.W., Guidotti, F.P. (1965). Painful heel: report of 323 patients with 364 painful heels. Clinical Orthopaedics and related Research, 39: 178-186.
- Gerster, J.C., Vischer, T.L., Bennani, A. et al. (1977). The painful heel. Comparative study in rheumatoid arthritis, ankylosing spondylitis, Reiter’s syndrome, and generalised osteoarthritis. Annals of the Rheumatic Diseases, 36: 343-348.
- Menz, H.B., Zammit, G.V., Landorf, K.B. et al. (2008). Plantar calcaneal spurs in older people: longitudinal traction or vertical compression? Journal of Foot & Ankle Research, 1:7.
- Sadat-Ali, M. (1998). Plantar fasciitis/calcaneal spur among security forces personnel. Military Medicine, 163: 56-57.
- Li, J., Muehleman, C. (2007). Anatomic Relationship of Heel Spur to Surrounding Soft Tissues: Greater variability than previously reported. Clinical Anatomy, 20: 950-955.
- Smith, S., Tinley, P., Gilheany, M. et al. (2007). The inferior calcaneal spur – Anatomical and histological considerations. The Foot, 17: 25-31.
- Kumai, T., Benjamin, M. (2002). Heel spur formation and the subcalcaneal enthesis of the plantar fascia. The Journal of Rheumatology, 29: 1957-1964.


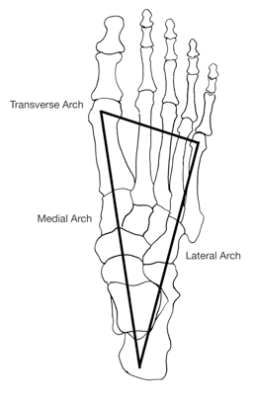
 As you can see one of the common findings seen in the research discussed has been that higher pressures are not seen beneath the 1st and 5th metatarsal heads during gait. Other authors have investigated this employing pressure measurement equipment and found that the pressures in the middle metatarsals are consistently greater than the 1st and 5th metatarsals.12,13 All of the research suggests that the tripod configuration of the foot is completely erroneous, and without this, it is obvious that it is not possible for there to be a transverse metatarsal arch. Clinicians who continue to talk about the transverse arch, and offer treatments for its ‘collapse’ are either uninformed, bogged down in old habits or in denial.
As you can see one of the common findings seen in the research discussed has been that higher pressures are not seen beneath the 1st and 5th metatarsal heads during gait. Other authors have investigated this employing pressure measurement equipment and found that the pressures in the middle metatarsals are consistently greater than the 1st and 5th metatarsals.12,13 All of the research suggests that the tripod configuration of the foot is completely erroneous, and without this, it is obvious that it is not possible for there to be a transverse metatarsal arch. Clinicians who continue to talk about the transverse arch, and offer treatments for its ‘collapse’ are either uninformed, bogged down in old habits or in denial.