Following a media frenzy in 2010, the concept of running barefoot came under rather close scrutiny. With respect to its potential long term risks/benefits the research is not yet available, so for many professionals the jury is still out and they remain healthily sceptical. However these same professionals generally recommend road running shoes based on a model which has been used for decades. At this point in time it seems only fair that this is re-visited and also put under the same scrutiny, with some of the available research relevant to running shoes looked at in closer detail. This blog aims to do just this; to discuss how road running shoes are currently ‘prescribed’, and to see if there is any rationale for this current practice.
History
Road running shoes can be generally split into 3 groups – motion control shoes, stability shoes, and neutral/cushioned shoes. Historically we have all been told that there are 3 main foot types (what a fantastic coincidence I hear you cry…) – the ‘flat’ or ‘pronated’ foot, the ‘normal’ or ‘neutral’ foot, and the ‘high arched’ or ‘supinated’ foot.

1. Flat/Pronated foot = Motion Control shoe 2. Normal/Neutral foot = Stability shoe 3. High/Supinated foot = Neutral/Cushioned shoe
It is not entirely clear where this model of shoe selection came from. It’s conception may have been based upon the work of Colonel Harris and Major Beath, who performed an Army foot survey back in 1947, and whilst doing so invented an ingenious new method of assessing footprints.1 It was in 1980 that ‘The Running Shoe book’ showed the first picture (as far as I’m aware) of the three arch types and how these may relate to running shoe selection.2 Despite the lack of certainty regarding its origins, pretty much every edition of Runners World magazine printed since has regurgitated this information, as have most running shoe shop assistants, not to mention numerous websites (including those of many major shoe companies and sports injury professionals). For several decades runners have therefore been advised to check their footprints (often easily assessed by observing the mark a wet foot leaves behind) and pick the corresponding shoe. They are told this ensures ideal alignment and minimises injury risk. Simples. Or is it?
Before we continue take a look at the following foot (a freeze frame during running):

Have a think about what running shoe you would recommend for this individual based on the visual information you have.
To identify whether the well known model of shoe selection is appropriate we need to break it down and analyse the preconceptions it is based upon. These are:
(A) Pronation is consistently predictive of injury.
(B) All individuals should be aligned identically (i.e. ‘normal’ or ‘neutral’).
(C) The wet foot test (i.e. foot shape) is predictive of dynamic function.
(D) Running shoe technology will actually achieve what it claims to.
If these points are not true, or not backed up by research, then the entire model falls apart. So, let’s take a look at these preconceptions one at a time.
(A) Pronation is consistently predictive of injury.
Running stores and magazines seem to be fixated on pronation. Most shoes are marketed with respect to how much ‘pronation control’ they offer. Why is this? Well, it has generally been thought that a more pronated foot type is a significant risk factor for injury. However the fact is that there are very few prospective studies which have actually shown this, with numerous studies actually concluding that there is no association between foot type and injury.3-9Two studies have even shown that a pronated foot is actually a protective factor against injury.10,11
The point I’m trying to make is that the relationship between foot mechanics and lower limb injury is still not as well understood as we think (or as we would like). But what we do know is that functioning in a pronated position does not mean that you will necessarily get injured. In fact the experimental evidence suggests you are much more likely to get injured from training errors12 or from dysfunctional hip musculature.13
Verdict = Pronation is not consistently predictive of injury
(B) All individuals should be aligned identically (i.e. ‘normal’ or ‘neutral’).
When referring to ‘ideal’ alignment what is actually meant? What exactly is ‘normal’ when it comes to the alignment of the lower extremity? Answer: We don’t know. The word ‘normal’ is probably an inappropriate word to apply to the human body. As far as normal foot alignment or mechanics is concerned, the normal (average) foot type reported in sampled populations is actually mildly to moderately pronated.14-17 So why then is the main aim of the current running shoe selection model to align runners to ‘neutral’ (i.e. the foot sitting perpendicular to the horizontal ground)?
When we consider that the subtalar joint (the joint where pronation and supination occurs) has variable anatomy 18,19it seems obvious that function will not be the same for everyone, and therefore that the ‘optimum’ position to be in would differ from person to person. Unsurprisingly, differences in foot alignment between individuals is reported to be high.20
It still amazes me that in a world where human variation is so vast in almost every aspect of our being, that when it comes to running there is a suggestion that we should all be in one particular alignment or position. The reality is that each of us most likely has own preferred alignment – a subject specific ‘normal’.
Verdict = Individuals should not all be aligned similarly. ‘Normal’ alignment is subject specific.
(C) The wet foot test (i.e. foot shape) is predictive of dynamic function.
The association between static foot measures and dynamic function has been well researched in the literature. Several different methods of assessing foot shape, arch height and foot posture in static standing have been investigated, with the conclusions generally being that there is no association between these measures and dynamic function (what the foot does when we actually run).21-25
The work which really puts the wet foot test out of business was completed by a team of researchers from the US army over the last year or so. Their prospective studies assigned running shoes based on plantar foot shape prior to basic military training, and investigated if this influenced injury risk at all. They showed that assigning running shoes based on the footprint shape had little influence on injury risk in Air Force Basic Training,26 Marine Corps Basic Training,27and Army Basic Combat Training.28
Verdict = Foot shape is NOT predictive of dynamic function. The wet foot test is nonsense.
(D) Running shoe technology will actually achieve what it claims to.
The technology that shoes provide can be generalised into 2 main areas. They offer cushioning, and market this as essential for the dampening of the high impacts associated with running, and they offer increased durometer (stiffer/harder) midsoles which are aimed at controlling or reducing pronation. These technologies have been called into question before, with some researchers suggesting that the protected environment a modern running shoe provides will diminish sensory feedback, resulting in inadequate impact moderating behaviour and actually serve to increase injury risk.29,30
A 2010 study concluded that the prescription of shoes with elevated cushioned heels and pronation control systems tailored to an individuals foot type was not evidence based31 and another very recent piece of research suggested this approach was overly simplistic and potentially injurious.32 How did the latter study come to this conclusion? Well to very briefly summarise: every single runner in their study who had been classified as having a ‘highly pronated’ foot type and was subsequently put into a motion control shoe reported an injury during a 13 week half marathon training programme. Let me repeat that – highly pronated feet that were put into motion control shoes resulted in injury. Yet that is exactly what the current shoe selection model suggests. So, let’s go back to the video gait analysis snapshot:

Given what you have read so far, what shoe would you recommend this person now? Has it changed from earlier?
Back to the running shoe research: Numerous studies agree that shoes with softer midsoles (cushioned/neutral shoes) result in greater pronation values, and shorter times to reach maximum pronation i.e. they make individuals pronate more, and pronate quicker.33-36 Does this sound bad to you? [If so go back and read the research which refutes preconception (A)]. Most of these studies also concluded that harder/stiffer midsoles (such as those found in stability and motion control shoes) significantly decrease the speed and magnitude of pronation. Some of these shoes now also have a slight varus tilt (they are higher on the inside of the heel than they are on the outside). Research has also shown that this decreases foot level pronation.37,38 (Remember these studies are just investigating kinematics/alignment and not injury).
So ‘anti-pronatory’ shoes with stiffer midsoles are actually doing what they promise to. The problem is we don’t know whether we need them to do it for us or not. And as an aside, varus posting/tilting was shown in one study to increase tibial shock and vertical loading rates.39 (Is this perhaps why all those injuries occurred in the motion control shoes in the aforementioned study?)
Finally, let’s not forget cushioning. That must reduce the amount of force we are subjected to when running – right? Wrong. As shoe cushioning decreases runners modify their patterns to maintain constant external loads.40 However, it is thought to contribute to comfort, and this seems to be the most important variable on which to select sports shoes, which we will talk about shortly.
Verdict = There is very little research investigating the relationship between running shoes and injury prevention. Stiffer midsoles do reduce pronation speed and magnitude, but in doing so may increase vertical loading rates. Running shoe ‘cushioning’ may be a myth.
Summary
It seems that the current model upon which running shoes are recommended/chosen is erroneous. Its foundations are based upon preconceptions which have been shown to be false. Due to significant within-species variation it is ridiculous to try and align people identically, (and to aim to do so in a pre-selected ‘normal’ position which is highly unlikely to be ‘normal’ for most individuals is potentially injurious). Shoes do seem to generally achieve what they claim to. However, our understanding of whether they actually need to achieve these variables (and who would benefit from each variable) is poor at present.
And so, the current method of being recommended a shoe still continues (and I imagine it will for some time). Why?
- Very few people realise it is erroneous.
- At the moment we do not have anything to replace it with.
- It is fantastically simple.
- People don’t generally like change.
The future
Moving forward, a much better model would be to focus on identifying an optimum midsole stiffness (which may be variable) for an individual, combined with their optimum alignment/movement patterns for a given activity (i.e. the position in which their injury risk is minimised and their performance is maximised, irrespective of its visual alignment). However, much more research is required before we fully understand how to clinically achieve this.
The concept of intelligent shoes which modify their midsole characteristics depending on the step by step requirements and effectively ‘tune’ themselves to the wearer and the surface they are on may sound like something from Back to the Future, but it is probably only a matter of time before we start seeing this sort of advancement in our running shoe technology. However, it doesn’t change the fact that we need a greater understanding of injury risk factors, and that these are still likely to be subject (and activity) specific.
Conclusions
So where does this leave the runner choosing a pair of shoes in 2011? There are many choices. Neutral? Stability? Motion Control? Vibram Five Fingers? Barefoot? Hopefully by now you realise that there is no simple answer.
All decisions could and should be based on one main factor in my opinion: comfort. Believe it or not comfort has been linked to injury frequency reduction41 and is thought to be the most important variable for sports shoes, and a focal point for any future sports shoe development.42 We all know that comfort is subjective and subject specific43 so with that in mind only the wearer can confidently choose the most appropriate shoe for themselves. [Be wary of the shop assistant/Podiatrist who tells you the exact make and model shoe which is best for you]. What one person finds comfortable will differ greatly from another; perhaps this is why some people find that stiff supportive shoes work best for them, and others discovered that barefoot running was the answer to their long history of injury woes.
As most runners know, it can often be a little bit of trial and error with regard to finding the ‘right’ shoe. Once you’ve found what works for you (or if you have found it already) then don’t change it.
Irrespective of the advice given in the shoe shop/magazines about your ‘pronation’; on current evidence you may be just as well off picking a shoe based on comfort alone, and subscribing to a course of Pilates and adopting sensible training habits.

P.S. How are you getting on with your decision on what shoes to recommend for this chap?
References
- Harris RI, & Beath T: (1947). Referenced from a secondary source: The Journal of Bone & Joint Surgery (1950), Vol 32B, No 1, p143-144.
- Cavanagh PR: The Running Shoe Book, Anderson World, Inc., Mountain View, California, 1980.
- Barrett JR, Tanji JL, Drake C, et al: High versus low-top shoes for the prevention of ankle sprains in basketball players. A prospective randomized study. The American Journal of Sports Medicine 21: 582, 1993.
- Twellaar M, Verstappen FT, Huson A, et al: Physical characteristics as risk factors for sports injuries: a four year prospective study. International Journal of Sports Medicine 18: 66, 1997.
- Wen DY, Puffer JC, Schmalzried TP, et al: Injuries in runners: a prospective study of alignment. Clinical Journal of Sport Medicine 8: 187, 1998.
- Beynnon BD, Renstrom PA, Alosa DM, et al: Ankle ligament injury risk factors: a prospective study of college athletes. Journal of Orthopaedic Research 19: 213, 2001.
- Hetsroni I, Finestone A, Milgrom C, et al: A prospective biomechanical study of the association between foot pronation and the incidence of anterior knee pain among military recruits. Journal of Bone and Joint Surgery Br88: 905, 2006.
- Reinking MF, Austin TM, Hayes AM: Risk factors for self-reported exercise-related leg pain in high school cross-country athletes. Journal of Athletic Training 45: 51, 2010.
- Franettovich M, Chapman AR, Blanch P, et al: Altered neuromuscular control in individuals with exercise-related leg pain. Medicine and Science in Sport and Exercise 42: 546, 2010.
- Giladi M, Milgrom C, Stein M, et al: The low arch, a protective factor in stress fractures. Orthopaedic Review 14: 81, 1985.
- Cowan D, Jones B, Robinson J: Foot morphologic characteristics and risk of exercise related injury. Archives of Family Medicine 2: 773, 1993
- James SL, Bates BT, Osternig LR: Injuries to runners. American Journal of Sports Medicine 6: 40, 1978.
- Ferber R, Hreljac A, Kendall KD: Suspected mechanisms in the cause of overuse running injuries: a clinical review. Sports Health: A Multidisciplinary Approach 1: 242, 2009.
- Sobel E, Levitz SJ, Caselli MA, et al: Re-evaluation of the relaxed calcaneal stance position. Journal of the American Podiatric Medical Association 89: 258, 1999.
- Scharfbillig R, Evans A, Copper A, et al: Criterion validation of four criteria of the foot posture index. Journal of the American Podiatric Medical Association 94: 31, 2004.
- Redmond A, Crosbie J, Ouvrier R: Development and validation of a novel rating system for scoring standing foot posture: the foot posture index. Clinical Biomechanics 21: 89, 2006.
- Redmond AC, Crane YZ, Menz HB: Normative values for the foot posture index. Journal of Foot and Ankle Research 1: 6, 2008.
- Bruckner J: Variations in the human subtalar joint. Journal of Orthopaedic and Sports Physical Therapy 8: 481, 1987.
- Forriol Campos F, Gomez Pellico L: Talar articular facets. Acta Anatomica 134: 124, 1989.
- Nester CJ: Lessons from dynamic cadaver and invasive bone pin studies: do we know how the foot really moves during gait? Journal of Foot and Ankle Research 2: 18, 2009.
- Razeghi M, Batt ME: Foot type classification: a critical review of current methods. Gait and Posture 15: 282, 2002.
- Hamill J, Bates BT, Knutzen KM, et al: Relationship between selected static and dynamic lower extremity measures. Clinical Biomechanics 4: 217, 1989.
- McPoil TG, Cornwall MW: The relationship between static lower extremity measures and rearfoot motion in gait. The Journal of Orthopaedic and Sports Physical Therapy 24: 309, 1996.
- Cashmere T, Smith R, Hunt A: Medial longitudinal arch of the foot: Stationary versus walking measures. Foot and Ankle International 20: 112, 1999.
- Trimble MH, Bishop MD, Buckley BD, et al: The relationship between clinical measurements of lower extremity posture and tibial translation. Clinical Biomechanics 17: 286, 2002.
- Knapik JJ, Brosch LC, Venuto M, et al: Effect on injuries of assigning shoes based on foot shape in air force basic training. American Journal of Preventative Medicine 38: S197, 2010.
- Knapik JJ, Trone DW, Swedler DI, et al: Injury reduction effectiveness of assigning running shoes based on plantar shape in marine corps basic training. American Journal of Sports Medicine 38: 1759, 2010.
- Knapik JJ, Swedler DI, Grier TL, et al: Injury reduction effectiveness of selecting running shoes based on plantar shape. Journal of Strength and Conditioning Research 23: 685, 2009.
- Robbins SE, Hanna AM: Running-related injury prevention through barefoot adaptations. Medicine and Science in Sports and Exercise 19: 148, 1987.
- Robbins SE, Gouw GJ: Athletic footwear: Unsafe due to perceptual illusions. Medicine and Science in Sports and Exercise 23: 217, 1991.
- Richards CE, Magin PJ, Callister R: Is your prescription of distance running shoes evidence-based? British Journal of Sports Medicine 43: 159, 2010.
- Ryan MB, Valiant GA, McDonald K, et al: The effect of three different levels of footwear stability on pain outcomes in women runners: a randomised control trial. British Journal of Sports Medicine (2010). doi: 10.1136/bjsm.2009.069849.
- Clarke TE, Frederick EC, Hamill CL: The effects of shoe design parameters on rearfoot control in running. Medicine and Science in Sports and Exercise 15: 376, 1983.
- Hamill J, Bates BT, Cole KG: Timing of lower extremity joint actions during treadmill running. Medicine and Science in Sports and Exercise 24: 807, 1992.
- Wit BD, Lenoir M: The effect of varying midsole hardness on impact forces and foot motion during foot contact in running. Journal of Applied Biomechanics 11: 395, 1995.
- Kersting UG, Bruggermann GP: Midsole material-related force control during heel-toe running. Research in Sports Medicine 14: 1, 2006.
- Van Woensel W, Cavanagh PR: A perturbation study of lower extremity motion during running. International Journal of Sports Medicine 34: 1844, 1992.
- O’Connor K, Hamill J: The role of selected extrinsic foot muscles during running. Clinical Biomechanics 19: 71, 2004.
- Perry SD, Lafortune MA: Influences of inversion/eversion of the foot upon impact loading during locomotion. Clinical Biomechanics 10: 253, 1995.
- Kong PW, Candelaria NG, Smith DR: Running in new and worn shoes: a comparison of three types of cushioning footwear. British Journal of Sports Medicine 43: 745, 2009.
- Mundermann A, Stefanyshyn DJ, Nigg BM: Relationship between footwear comfort of shoe inserts and anthropometric and sensory factors. Medicine and Science in Sports and Exercise 33: 1939, 2001.
- Nigg BM: Biomechanics of Sports Shoes, Topline Printing Inc, Calagary, Alberta, Canada, 2010.
- Miller JE, Nigg BM, Liu W, et al: Influence of foot, leg and shoe characteristics n subjective comfort. Foot and Ankle international 21: 759, 2000.




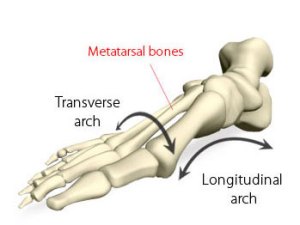
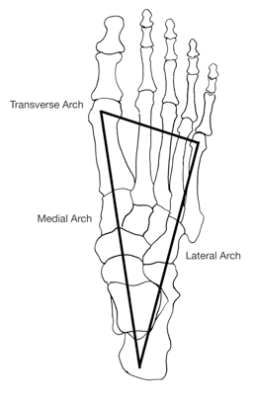
 As you can see one of the common findings seen in the research discussed has been that higher pressures are not seen beneath the 1st and 5th metatarsal heads during gait. Other authors have investigated this employing pressure measurement equipment and found that the pressures in the middle metatarsals are consistently greater than the 1st and 5th metatarsals.12,13 All of the research suggests that the tripod configuration of the foot is completely erroneous, and without this, it is obvious that it is not possible for there to be a transverse metatarsal arch. Clinicians who continue to talk about the transverse arch, and offer treatments for its ‘collapse’ are either uninformed, bogged down in old habits or in denial.
As you can see one of the common findings seen in the research discussed has been that higher pressures are not seen beneath the 1st and 5th metatarsal heads during gait. Other authors have investigated this employing pressure measurement equipment and found that the pressures in the middle metatarsals are consistently greater than the 1st and 5th metatarsals.12,13 All of the research suggests that the tripod configuration of the foot is completely erroneous, and without this, it is obvious that it is not possible for there to be a transverse metatarsal arch. Clinicians who continue to talk about the transverse arch, and offer treatments for its ‘collapse’ are either uninformed, bogged down in old habits or in denial.